
7 Essential Insights into Asherman’s Syndrome
An Academic Perspective on Uterine Health
Asherman’s Syndrome is a gynecological condition that involves the formation of intrauterine adhesions, significantly affecting uterine health and fertility. This article provides a clear and accessible overview of Asherman’s Syndrome, exploring its causes, symptoms, diagnostic methods, and treatment strategies. Understanding this condition is essential for students, professionals, and anyone interested in reproductive health.
Asherman’s Syndrome: Defining Intrauterine Adhesions
The uterus, a remarkable muscular organ, is anatomically designed to facilitate gestation. Its inner lining, the endometrium, undergoes monthly proliferative and secretory phases in preparation for potential embryonic implantation. In the absence of pregnancy, this functional layer is shed, resulting in menstruation.
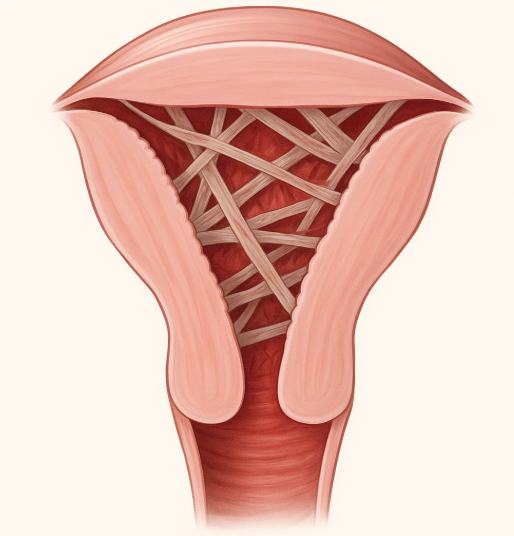
Asherman’s Syndrome, also known as Intrauterine Adhesions (IUAs) or uterine synechiae, is characterized by the formation of scar tissue within the uterine cavity. This fibrotic tissue can vary in density and extent, ranging from thin, easily separable adhesions to thick, dense, and confluent bands that can partially or completely obliterate the uterine lumen. Such adhesions can distort the normal uterine architecture, impairing its physiological functions. The syndrome was first extensively described by Dr. Joseph G. Asherman in the mid-20th century, highlighting its historical recognition within gynecology. Despite its significant impact on reproductive health, the prevalence of Asherman’s Syndrome may be underestimated due to varied diagnostic practices and asymptomatic presentations in milder cases.
Etiology of Asherman’s Syndrome: Understanding the Causes
The development of Asherman’s Syndrome is predominantly iatrogenic, stemming from trauma to the basal layer of the endometrium. The most frequent causative factor is an aggressive or repeated surgical procedure performed within the uterine cavity.
- Dilation and Curettage (D&C): This procedure, involving the dilation of the cervix and subsequent mechanical removal or suction of uterine tissue, is a primary contributor to IUA formation. D&C is commonly performed following miscarriage, elective abortion, or for the evacuation of retained products of conception postpartum. While generally safe, this procedure carries a risk of endometrial basal layer injury, leading to an aberrant healing process and subsequent adhesion formation, which can culminate in Asherman’s Syndrome.
- Postpartum Complications: Retained placental fragments after childbirth can necessitate a D&C, indirectly increasing the risk of Asherman’s Syndrome. Additionally, severe postpartum hemorrhage requiring uterine exploration may also contribute to endometrial trauma.
- Other Uterine Surgeries: Procedures such as myomectomy (surgical removal of uterine fibroids), particularly those involving hysteroscopic resection or extensive uterine wall incision, or even certain cesarean sections, can, in rare instances, predispose to IUA formation through direct endometrial damage.
- Infections: Although less common as a sole cause, severe intrauterine infections, such as endometritis, can lead to significant endometrial inflammation and subsequent scar tissue development during the healing phase, potentially resulting in Asherman’s Syndrome.
It is crucial to recognize that the occurrence of these procedures does not guarantee the development of Asherman’s Syndrome. The risk is influenced by factors such as the extent of endometrial trauma, the presence of infection, and individual healing responses.
Clinical Manifestations and Diagnostic Approaches for Asherman’s Syndrome
The presentation of Asherman’s Syndrome is varied, primarily affecting menstrual patterns and reproductive capability. Identifying the condition relies on a combination of clinical suspicion and targeted diagnostic imaging.
- Menstrual Irregularities: A hallmark symptom is a significant change in menstrual flow, often presenting as hypomenorrhea (scanty periods), oligomenorrhea (infrequent periods), or amenorrhea (complete absence of menstruation). This reduction in flow directly correlates with the decreased functional endometrial surface area due to scarring.
- Infertility and Recurrent Pregnancy Loss: The distorted uterine cavity and impaired endometrial receptivity can hinder successful embryonic implantation and subsequent gestational development, making Asherman’s Syndrome a significant cause of secondary infertility and recurrent miscarriages.
- Pelvic Pain: In cases where adhesions occlude the cervical canal, menstrual blood can become entrapped within the uterus (hematometra), leading to cyclic or chronic pelvic pain and discomfort.
Definitive diagnosis of Asherman’s Syndrome requires specialized imaging techniques:
- Hysteroscopy: Considered the gold standard, hysteroscopy involves the direct visualization of the intrauterine cavity using a thin, lighted telescope inserted through the cervix. This allows for precise identification, classification, and mapping of the adhesions, assessing their type, extent, and location.
- Hysterosalpingography (HSG): This radiographic procedure involves injecting a contrast dye into the uterus and fallopian tubes. Under X-ray fluoroscopy, the dye’s flow pattern can reveal filling defects, irregular contours, or partial/complete obliteration of the uterine cavity, indicative of IUAs characteristic of Asherman’s Syndrome.
Therapeutic Strategies for Asherman’s Syndrome
Asherman’s Syndrome is a treatable condition, with the primary objective being the meticulous removal of scar tissue and restoration of normal uterine anatomy and function.
- Hysteroscopic Adhesiolysis: The principal therapeutic intervention for Asherman’s Syndrome is hysteroscopic adhesiolysis. Utilizing the hysteroscopic system, a surgeon can carefully resect or vaporize the adhesions using micro-scissors, electrosurgical instruments, or laser fibers. This delicate procedure aims to meticulously separate the fibrotic bands while preserving the remaining healthy endometrium.
- Post-Operative Management to Prevent Re-adhesion: Following adhesiolysis, there is a risk of re-formation of adhesions. To mitigate this, several strategies are employed:
- Intrauterine Balloon or Stent Placement: A small balloon catheter or a similar device may be temporarily placed within the uterine cavity for several days or weeks to physically separate the uterine walls during the initial healing phase.
- Hormonal Therapy: High-dose estrogen therapy, often followed by a progestin, is commonly prescribed post-operatively to stimulate endometrial regeneration and promote healthy re-epithelialization, thereby reducing the likelihood of new adhesion formation.
- Anti-Adhesion Barriers: Various agents, such as hyaluronic acid gels or oxidized regenerated cellulose, can be applied to the uterine cavity to create a temporary barrier between the healing surfaces.
- Intrauterine Device (IUD) Placement: In some protocols, a non-hormonal IUD may be temporarily inserted to act as a physical barrier against re-adhesion.
The success of treatment is influenced by the initial severity and extent of the adhesions. While milder cases often achieve excellent anatomical and functional restoration, severe cases may require multiple procedures and present a greater challenge, though significant improvements in symptoms and reproductive outcomes are frequently observed for patients with Asherman’s Syndrome.
Proactive Measures and Prognosis for Asherman’s Syndrome
While Asherman’s Syndrome poses a challenging clinical scenario, heightened awareness and meticulous surgical techniques can contribute to prevention. Healthcare providers performing intrauterine procedures are encouraged to utilize hysteroscopic guidance to minimize endometrial trauma. For individuals undergoing such procedures, open communication with their physician regarding potential risks and preventative strategies is advisable.
For those diagnosed with Asherman’s Syndrome, it is important to emphasize that effective treatments exist. Ongoing advancements in gynecological surgery and reproductive medicine continue to improve outcomes, enabling many individuals to experience resolution of symptoms and achieve successful pregnancies after appropriate intervention. Understanding one’s own physiology and actively engaging in health advocacy are paramount in navigating such conditions.
Conclusion: Advancing Understanding in Gynecological Health
This exploration of Asherman’s Syndrome underscores the importance of comprehending specific gynecological conditions that can significantly impact reproductive health. By delving into its causes, diagnostic methods, and therapeutic strategies, we aim to contribute to a more informed perspective on uterine health. Such knowledge not only empowers individuals but also fosters a deeper appreciation for the complexities and resilience of the human body. Continued inquiry and dissemination of accurate medical information are vital for advancing health literacy and improving patient outcomes in the field of gynecology. For further reading, consider exploring our article on [link interno a otro artículo relevante, e.g., “Understanding Endometriosis”].
Glosario:
- Endometrium: The inner mucosal lining of the uterus.
- Adhesions: Fibrous bands of scar tissue, specifically intrauterine adhesions (IUAs) when located within the uterine cavity.
- Dilation and Curettage (D&C): A surgical procedure involving the dilation of the cervix and the scraping or suctioning of the uterine lining.
- Amenorrhea: The absence of menstruation.
- Hysteroscopy: An endoscopic procedure to directly visualize the interior of the uterus.
- Hysterosalpingography (HSG): A radiological procedure utilizing contrast dye to evaluate the patency of the fallopian tubes and the morphology of the uterine cavity.
- Hysteroscopic Adhesiolysis: A surgical procedure performed via hysteroscopy to excise or ablate intrauterine adhesions.
References:
- Queckbörner S, Davies LC, von Grothusen C, Santamaria X, Simón C, Gemzell-Danielsson K. Cellular therapies for the endometrium: An update. Acta Obstet Gynecol Scand. 2019
- Guo EJ, Chung JPW, Poon LCY, Li TC. Reproductive outcomes after surgical treatment of asherman syndrome: A systematic review. Best Pract Res Clin Obstet Gynaecol. 2019
- Ludwin A, Martins WP, Ludwin I. Ultrasound-guided repeat intrauterine balloon dilatation for prevention of adhesions. Ultrasound Obstet Gynecol. 2019
- Chikazawa K, Imai K, Liangcheng W, Sasaki S, Horiuchi I, Kuwata T, Takagi K. Detection of Asherman’s syndrome after conservative management of placenta accreta: a case report. J Med Case Rep. 2018
- Al-Inany H. Intrauterine adhesions. An update. Acta Obstet Gynecol Scand. 2001 Nov;80(11):986-93.
- Tchente NC, Brichant G, Nisolle M. [Asherman’s syndrome : management after curettage following a postnatal placental retention and literature review]. Rev Med Liege. 2018 Oct;73(10):508-512.
- ASIMAKOPULOS N. TRAUMATIC INTRAUTERINE ADHESIONS. (THE FRITSCH-ASHERMAN SYNDROME). Can Med Assoc J. 1965 Aug 14;93(7):298-302.
- Young BK. A multidisciplinary approach to pregnancy loss: the pregnancy loss prevention center. J Perinat Med. 2018 Dec 19;47(1):41-44.
- Capmas P, Pourcelot AG, Fernandez H. Are synechiae a complication of laparotomic myomectomy? Reprod Biomed Online. 2018 Apr;36(4):450-454.
- Dreisler E, Kjer JJ. Asherman’s syndrome: current perspectives on diagnosis and management. Int J Womens Health. 2019;11:191-198.
- Azizi R, Aghebati-Maleki L, Nouri M, Marofi F, Negargar S, Yousefi M. Stem cell therapy in Asherman syndrome and thin endometrium: Stem cell- based therapy. Biomed Pharmacother. 2018 Jun;102:333-343.
🔍 Interested in learning more about gynecology and reproductive health?
Check out these related articles:

Leave a Reply